Panel Members’ Handbook 2013
Table of Contents
- Foreword
- Chapter 1: Acronyms and Definitions
- Chapter 2: Legislation related to the Immigration Medical Examination (IME)
- Chapter 3: The Work of Panel Members
- 3.1 Responsibilities
- 3.1.1 General
- 3.1.2 Consultant or specialist referrals
- 3.1.3 eMedical responsibilities
- 3.1.4 Performance guidelines
- 3.1.5 Conflict of interest and ethical responsibilities
- 3.1.6 Fraud prevention
- 3.1.7 Cultural sensitivities
- 3.1.8 Performance evaluation
- 3.1.9 Absences from IME activities
- 3.1.10 Locum tenens
- 3.1.11 Official languages
- 3.1.12 Use of interpreters
- 3.2 Unique identifiers for panel members
- 3.3 Guidelines for records management
- 3.4 Administrative instructions
- 3.4.1 Communication with the regional medical offices
- 3.4.2 Advertising
- 3.4.3 Issues not related to immigration medical activities
- 3.4.4 Communication with the media
- 3.4.5 Communication issues related to clients
- 3.4.6 Enquiries about completing an IME
- 3.4.7 General eMedical system enquiries
- 3.4.8 Fees for IME
- 3.4.9 Incidents, complaints and quality assurance concerns
- 3.4.10 Resolution process for complaints or performance issues
- 3.1 Responsibilities
- Chapter 4: Immigration Medical Examination (IME)
- 4.1 Verification of identity
- 4.2 Client Consent and Declaration (IMM 5743)
- 4.3 Medical Report: Client Biodata and Summary (IMM 1017)
- 4.4 IME grading
- 4.5 Panel physician declaration
- 4.6 Medical History (IMM 5419)
- 4.7 Physical Examination (IMM 5419)
- 4.8 Laboratory Requisition and Report
- 4.9 Chest X-Ray Requisition and Report
- 4.10 Furtherance process
- 4.11 Additional forms and information
- Chapter 5: Panel Members’ Activities in Canada
- Appendix I: Contact Information
- Appendix II: Client Consent and Declaration
- Appendix III: Forms
- IMM 1017: Upfront Medical Report – Client Biodata and Summary
- IMM 1017B Upfront: Upfront Medical Report – Client Biodata and Summary
- IMM 5419: Medical Report
- IMM 5544: Resettlement Needs Assessment Form
- IMM 5725: Activities of Daily Living
- IMM 5727: Global Assessment of Functioning
- IMM 5728: Acknowledgment of HIV Post-Testing Counselling
- IMM 5733: Instructions for Pregnant Client − X-Ray Deferred
- IMM 5734: Specialist’s Referral Form
- IMM 5738: Chart of Early Childhood Development
- IMM 5965: Important Medical Information - Syphilis Treatment Form
- Appendix IV: List of Immigration Medical Examination Instructions (IMEIs)
- Appendix V: Instructions for Submission of Paper-Based IME
Foreword
Citizenship and Immigration Canada’s (CIC) Health Branch is responsible for the administration and delivery of the Department’s health programs. These responsibilities include management of the panel members (including panel physicians, panel radiologists and laboratories) who perform immigration medical examinations (IMEs) in Canada and abroad.
CIC provides immigration medical services through six regional medical offices (RMOs). In providing these services, the RMOs rely on the IMEs that panel members conduct on clients for permanent residency and some categories of temporary residency in Canada. Health findings on the IMEs allow CIC medical officers to make recommendations on the medical admissibility of persons requesting entry to Canada.
In order to modernize how it conducts its business, CIC is committed to simpler, more accessible services; to continuous, innovative and adaptable operational improvement; and to robust program integrity and delivery of quality service. As part of its modernization agenda, CIC has implemented an electronic IME Web-based processing system called eMedical. eMedical is a joint Canada-Australia information technology project that will result in significant savings in processing time, strengthen overall program integrity, and provide many other benefits for clients, panel members and CIC. Panel members working in countries where eMedical is implemented will need to complete and transmit all IMEs through this Web-based system.
This Handbook provides instructions, information and reference material related to the work of panel members and to the IME process. Panel members may include physicians, radiologists, laboratories and other designated health care professionals involved in the IME process. Together, they make up CIC’s network of panel members.
You can visit the Department’s website at cic.gc.ca for further information on Canada’s immigration program.
Issues affecting the health of immigrants and the immigration process itself are subject to change. Periodic updates of this Handbook will be issued when required. These updates will supersede the text they replace. In all cases, the online version of the Handbook will be the most current and is the version that should be consulted.
Chapter 1: Acronyms and Definitions
The following list provides definitions for acronyms and technical terms found in this Handbook:
- ADL
- Activities of daily living
- Biodata
- Information that establishes each client’s identity
- CECD
- Chart of Early Childhood Development
- CIC
- Citizenship and Immigration Canada
- Client
- A foreign national who is seeking to enter Canada, and in accordance with the Immigration and Refugee Protection Act and its Regulations, is required to submit to an IME.
- Clinic staff
- Persons who are working in the panel member’s clinic and may be involved in the immigration medical process.
- CXR
- Chest x-ray
- DIAC
- Department of Immigration and Citizenship (Australia)
- DICOM
- Computer disk with x-ray image
- DOT
- Directly observed therapy
- ED
- Excessive demand, i.e., a demand placed by a client on Canadian health or social services.
- EDE
- Excessive demand exempt is a category of client who is exempt from assessment of excessive demand.
- ELISA
- Enzyme-linked immunosorbent assay, also known as enzyme immunoassay, which is a blood test for HIV.
- eMedical
- An online application that provides a paperless process for electronic recording, transmission and storage of immigration health examination results.
- Furthered cases
- Cases that require supplemental medical reports to complete the medical assessment.
- GAF
- Global assessment of functioning
- Guardian
- A legal guardian is a person who has custody or who is empowered to act on behalf of another person and has been recognized as such by the competent authorities in the jurisdiction where the status was either recognized or granted.
- Handbook
- This Handbook is the standard reference for the orientation and training of panel members. All panel members must ensure that they remain familiar with it and with departmental instructions, including interim changes and updates provided by CIC.
- HIV
- Human immunodeficiency virus
- IFHP
- Interim Federal Health Program: a program funded by CIC that provides limited, temporary coverage of costs related to health care for specific categories of people, including protected persons, refugee claimants, rejected refugee claimants, certain persons detained under the Immigration and Refugee Protection Act (IRPA) and other specified groups.
- IMA
- Immigration medical assessment, i.e., the medical determination made by a CIC edical officer of a client’s admissibility to Canada.
- IME
- Immigration medical examination: the examination is conducted by a panel member. The results of these examinations are sent to CIC medical officers who conduct IMAs.
- IME number
- Immigration medical examination number
- IMEIs
- Immigration medical examination instructions, i.e., the instructions for completion of the IME.
- IMM 0535
- Medical Surveillance Undertaking Form, issued to individuals who have undergone their IME in Canada or abroad and have been determined to require medical surveillance by Canadian Public Health Authorities.
- IMM 1017
- An IME form containing the client’s biodata, IME grading and panel physician declaration.
- IMM 5419
- An IME form containing the client’s medical history, physical examination findings, laboratory, chest x-ray requisition results and the client’s consent and declaration.
- IMM 5544
- Supplemental medical and resettlement needs assessment form providing information on the special needs a client may have while settling in Canada.
- IOM
- International Organization for Migration
- IRPA and IRPR
- Immigration and Refugee Protection Act and the Immigration and Refugee Protection Regulations, i.e., Canadian federal legislation setting out the requirements for immigrating to or visiting Canada, including the requirement to have an IME and be medically admissible. The Act and Regulations can be found at http://laws-lois.justice.gc.ca/eng/acts/I-2.5/.
- LFT
- Liver function test
- Locum tenens
- Medical practitioners who replace panel physicians for a short period while they are on vacation, taking training or unable to provide service for other reasons.
- LTBI
- Latent tuberculosis infection
- Panel clinic
- A clinic where designated physicians and radiologists conduct IMEs.
- Panel member
- A general term that refers to a panel physician, panel radiologist or panel laboratories or specialists authorized by CIC to perform IME-related activities.
- Panel physician
- New term used for a medical doctor designated to perform, grade and submit IMEs. Designated medical practitioner (DMP) was the previously used term.
- Panel radiologist
- A radiologist designated to perform, grade and submit chest x-rays for IMEs.
- P number
- A unique identifier for each panel member issued by the Health Branch.
- PHLU
- Public Health Liaison Unit, located in the Health Branch, CIC (the former term was Medical Surveillance Unit).
- Protected person – In Canada
- People who have been determined to be protected persons by the Immigration and Refugee Board of Canada (IRB), or in a Pre-Removal Risk Assessment, and who have been granted permanent residence as a result.
- PTB
- Pulmonary tuberculosis
- PTC
- Post test counselling
- Refugee overseas
- Convention refugee overseas
- RMO
- Regional medical office is the location of operations for medical officers who are CIC officials with responsibility for the Canadian immigration health program in a given region.
- TB
- Tuberculosis
- TST
- Tuberculin skin test
- UCI
- Unique client identifier
- UFM
- Upfront medical
- UMI
- Unique medical identifier
- VDRL
- Venereal Disease Research Laboratory test, which is a blood test for syphilis.
- VO
- Visa office, where immigration and other applications are processed.
- WHO
- World Health Organization
Chapter 2: Legislation related to the Immigration Medical Examination
Immigration is a shared federal/provincial responsibility. Panel members should be aware of the following legislation as it relates to immigration and the requirements with respect to medical examinations and inadmissibility on health grounds.
2.1 Immigration and Refugee Protection Act
The Immigration and Refugee Protection Act (IRPA) is a federal act. One of the objectives is to ensure that the movement of people into Canada contributes to the country’s cultural, social, and economic interests and affirms its humanitarian commitments, while protecting the health, safety and security of Canadians.
The IRPA and its accompanying regulations set out the medical requirements that clients must meet in order to come to Canada as temporary or permanent residents.
In addition, the legislation sets out the grounds on which a person may be found to be inadmissible to Canada, including inadmissibility on health grounds.
A foreign national is inadmissible on health grounds if his/her health condition:
- is likely to be a danger to public health;
- is likely to be a danger to public safety; or
- might reasonably be expected to cause excessive demand on health or social services.
The IRPA may be viewed at http://laws-lois.justice.gc.ca/eng/acts/I-2.5/index.html.
2.2 Privacy Act
The purpose of this Act is to protect the privacy of individuals with respect to personal information collected by the government and to provide individuals with a right of access to their personal information.
The Privacy Act may be viewed at http://laws-lois.justice.gc.ca/eng/acts/P-21/index.html.
2.2.1 Disclosure of personal information under the Privacy Act
Under the Privacy Act, all individuals have the right to the protection of their personal information held by a federal institution. Moreover, Canadian citizens, permanent residents and other individuals present in Canada have the right of access to their own personal information held by government institutions.
Disclosure of personal information is governed by section 8 of the Privacy Act. Subsection 8(1) states that the government institution shall not disclose personal information without the consent of the individual to whom the information relates except under the circumstances provided under subsection 8(2).
Pursuant to paragraph 8(2)(f) of the Privacy Act, Health Branch has concluded Memoranda of Understanding with certain partner countries on information sharing in order to align our network of panel members, which allows Health Branch to share information about our network with partner countries. Health Branch requests that all panel physicians sign a consent form to share information with other immigration health authorities. The information to be shared will not be related to individual clients or a specific type of care; rather it will be generic information concerning administrative (such as email, contact addresses) and operational activities (such as electronic capabilities, locations) as well as information gathered during evaluations, assessments or onsite visits by CIC officers.
2.3 Access to Information Act
The Access to Information Act gives every Canadian citizen, permanent resident and individual or corporation present in Canada the right to access records, in any format, held by a government institution, subject to certain exceptions. The Access to Information Act may be viewed at http://laws-lois.justice.gc.ca/eng/acts/A-1/index.html.
The Act is used to access information held by the government apart from an individual’s own personal information. A client’s family or representatives in Canada often use the Act, with the client’s permission, to request information about the client’s immigration medical file.
It is not necessary for clients to use the Act to obtain a copy of the results of their own IME. Panel physicians are authorized to provide clients with a copy of their own IME upon the clients’ request.
Chapter 3: The Work of Panel Members
A panel member cannot be designated until all the requirements of the designation process have been met:
- Completion of all required forms:
- application form;
- consent to share information;
- consent to use eMedical where available;
- acknowledgment of having read the Handbook; and
- acceptance of designation.
- Provision of all required documents, such as proof of professional licence, certification and resumé;
- Completion of orientation, which includes reading and understanding this Handbook and participating in discussions with CIC medical personnel. Panel members are not authorized to perform IMEs for CIC during the orientation phase; and
- Completion of training, including eMedical training where and when relevant, which may be done individually or through group activities involving several panel members in locations where they operate in geographic proximity.
Once all forms and documents are received, the regional medical office (RMO) advises the panel member that he/she is approved as a panel member and a unique identifier number is provided.
Designation is not a permanent status and completing the designation process does not create any contract or agency relationship with CIC. A panel member’s designation may be terminated on 30 days’ notice.
CIC does not guarantee that you will receive a specific number of cases per year.
CIC immigration officials and medical officers consult one another regularly in order to determine the number of panel members required in a given location. Based on CIC’s operational requirements, the number of designated panel members in any given location may be reduced or increased.
If a panel member relocates his or her practice, that relocation must be brought to the attention of the RMO, as designation as a panel member is related to your location. Panel member status may be revoked because of the relocation. Upon examination of the new location of the practice and an assessment of the operational requirement for panel members in that location, the affected panel member will be informed of a decision confirming his or her status and given an opportunity to respond.
Complaints or disputes regarding a panel member’s performance may result in termination, depending on the situation. Sections 3.1.8, 3.4.9, and 3.4.10 of this chapter provide additional information on performance evaluations, complaints and the resolution process.
3.1 Responsibilities
Panel members, depending on their field of work, are authorized to perform IMEs, arrange for diagnostics and investigations, and complete immigration medical forms. They do not have the authority to assess or determine whether the medical conditions of clients are grounds for inadmissibility. More specifically, panel members do not have authority to give clients an opinion on their medical admissibility. That determination rests solely with Canadian immigration officers.
Panel members performing IMEs should ensure that they meet CIC-mandated service standards and that there are no conflicts of interest in providing services. They are also required to help prevent fraud and abuse of Canada’s immigration laws, submit to performance evaluations, follow proper procedures for absences, and use English or French in their communications with CIC.
For all clients, the Canadian IME will include an examination by a panel member and a medical assessment by a CIC medical officer. Where necessary to establish compliance with the IRPA and the Immigration and Refugee Protection Regulations, clients will be asked to undergo further medical examinations.
The assessment of whether or not a client is inadmissible on health grounds is based on the health findings identified during the examination by a panel member. This process is called the immigration medical assessment (IMA).
3.1.1 General
All panel members are required to:
- maintain familiarity with the latest version of this Handbook and all associated administrative and IME instructions;
- follow instructions regarding verification of the client’s identity;
- hold current professional registration and licensing issued by local or national regulatory authorities and provide proof thereof when requested by the RMO;
- maintain the confidentiality of all immigration medical information in their control and store that information securely;
- ensure that the fees charged for immigration medical services fairly represent the services performed and comply with local guidelines or those of a medical association or group;
- ensure that a list of fees and charges for the IME and related expenses is posted in the clinic or office. The list should include fees for required radiological and laboratory investigations, for postage or courier charges, and for other services. Any special fees for groups or large families should also be listed. Copies should be available for clients on request and all clients should receive a receipt for services;
- ensure that all panel clinic staff members under their supervision are aware of the requirements and standards for the IME and its procedures;
- ensure that panel clinic staff understand the role and obligations that pertain to panel members;
- ensure that individual and clinic contact information is up-to-date. eMedical users must keep their contact information updated in the system, while those who use paper-based forms must inform the RMO of changes in contact information; and
- ensure high quality of work by all professionals involved in conducting IMEs, including staff members and specialist consultants.
Panel physicians must:
- obtain client consent and declaration (see details in Section 4.2 and in Appendix II);
- follow their country’s public health regulations for notification of conditions of public health concern, such as tuberculosis (TB), syphilis, Human immunodeficiency virus (HIV) and hepatitis;
- conduct a complete IME, including physical and mental examinations, routine tests and appropriate pre- and post-test counselling for clients who undergo HIV testing, according to Health Branch immigrant medical examination instructions (IMEIs) (see links for each IMEI in Appendix IV); and
- coordinate all the IME results and the IME report to be submitted to CIC, including lab results and chest x-rays as well as reports from referred consultants and specialists when required by CIC.
Panel radiologists must:
- conduct chest x-rays (postero-anterior view only) according to the Canadian Association of Radiologists’ quality standards;
- complete the “special finding” form in order to grade the chest x-ray; and
- inform the panel physician of all suspected cases of active TB so that further investigations may be undertaken by the panel physician.
Panel laboratories:
Until laboratories are designated by CIC, panel physicians are responsible for ensuring that the laboratories they use:
- are aware of the requirements and standards for the Canadian IME;
- are in good standing and hold current registration and licensing issued by local or national regulatory authorities and can provide proof thereof when requested by the RMO;
- follow instructions for verifying the client’s identity described in Section 4.1; and
- comply with administrative requirements (see Section 3.4 below) and complete the “Laboratory Requisition and Report” section of the IMM 5419 accurately and prevent fraudulent substitution.
Once CIC has designated a laboratory in your area, panel physicians will be required to use this facility.
3.1.2 Consultant or specialist referrals
Panel physicians should ensure that:
- consultants, specialists and facilities providing supplemental tests understand that the request for additional information is only for a medical evaluation in the immigration process, and not for therapeutic purposes or to establish fitness to fly;
- consultants or specialist practitioners are currently registered, certified or licensed by national regulatory bodies; and
- consultants and other practitioners are aware of CIC’s requirements, particularly regarding verification of the client’s identity.
3.1.3 eMedical responsibilities
The eMedical system is a Web-based system implemented by CIC and the DIAC for the electronic recording and transmission of IMEs. In regions where eMedical is available, panel members and their clinic staff will be required to complete all IMEs and enter the results in the eMedical system, unless otherwise specified by the responsible RMO.
Where eMedical is available, all panel members are required to:
- complete and submit all IMEs and related documents through the eMedical system;
- maintain and keep secure their eMedical account, including user ID, password, and secret questions and answers;
- notify CIC immediately if their password becomes known by an unauthorized person;
- ensure that their personal and business information in the system is updated and accurate at all times;
- take all reasonable steps to guarantee the security of clients’ personal information contained in eMedical;
- ensure that clients’ personal information contained in eMedical is treated in a manner consistent with Canadian privacy laws. This includes, but is not limited to, protecting collected information against loss and unauthorized access, use, modification, disclosure and other misuse; and
- ensure that all panel clinic staff under their supervision are aware of and abide by the requirements and standards for completing IMEs in the eMedical system.
| Activities | Time frame (in calendar days) | |
|---|---|---|
| Appointment with panel physician, including cases where client is furthered | 14 days; for upfront medicals, within 2 business days | |
| Obtain lab results | 7 days after date of the exam | |
| Obtain x-ray results | 7 days after date of the exam | |
| Submission of the IME to RMO by the panel physician | 10 days of date of the exam | |
| Responding to correspondence from RMO | 48 hours | |
| Forwarding inactive immigration medical files to the RMO | Paper-based: 8 week old IMEs | eMedical users: Files are auto deleted after 365 days of inactivity |
| Notifying the responsible RMO of any change in practice location or contact information | At least 14 days before the change takes place | |
| Notifying the responsible RMO of any absence of 7 days or more | At least 14 days’ notice, (preferably by email) | |
| Being available for RMO visits and for provision of performance and technical information related to the IME process (e.g., quality assurance visits, annual audits) | 7 days notice | |
3.1.5 Conflict of interest and ethical responsibilities
- Panel members may become involved in situations where their loyalties are divided or the client’s personal interests conflict with the panel member’s responsibilities. Panel members are expected to exhibit professional behaviour and perform their IME-related activities in a manner that is in keeping with the principles of proper medical practice and with CIC policy.
- Panel physicians are to provide appropriate and timely advice to the client when they discover a serious disease not known to the client.
- In doing so, they are to uphold professional and ethical standards by referring back to the client’s usual physician or to an appropriate specialist, upon request.
- If the following issues or events arise, panel members must notify the responsible RMO immediately:
- The panel member is suspended, or comes under investigation by his or her respective medical or regulatory authorities, or is charged, or convicted of a criminal offence or offences by medical or regulatory authorities; and/or
- The panel member discovers inappropriate activity relative to the provision of IMEs by clinic, office, laboratory or radiology centre staff.
Depending on the event reported, CIC may suspend designation (refer to Section 3.4.10) pending results of the investigation by the medical or regulatory authorities.
3.1.6 Fraud prevention
To support fraud prevention and the integrity of the IME process, panel members must confirm the identity of the client using an identification document acceptable for the Canadian Immigration medical examination. All documents must be valid ( not expired).
Approved identification documents include the following:
- Original passport or a copy of passport certified by a Canadian Visa Office
- National ID card (an original Birth Certificate is an acceptable national ID document for minors under the age of consent only.)
- Driver’s licence (in Canada only)
- Refugee travel document
- Red Cross travel document
- United Nations (UN) laissez-passer
- Seaman’s book
- Organization of American States travel document
- Refugee Protection Claimant Document
If personal details, including the photograph, are inconsistent with the identity documents submitted, panel members must inform CIC (see Section 4.1.3 for additional information).
Panel members or clinic staff must also inform CIC if they suspect that clients are providing false information or attempting to falsify any aspect of the IME.
Panel members can proceed with the IME, and CIC will follow up on the concern raised about the individual’s identity and any other report of possible fraud.
Panel members should help prevent fraud by educating their staff on procedures used to verify client identity (refer to Section 4.1 for additional information).
3.1.7 Cultural sensitivities
Panel members must be aware that clients from some cultures may request special accommodation during the IME. Female clients, for example, may be uncomfortable with a male examiner, in which case panel members should offer to have a chaperone present during the examination.
Panel members should try to accommodate personal and cultural sensitivities, while keeping in mind that IME standards must be respected. In such cases, panel members will indicate on the examination form the type of accommodation provided and the names of other persons present during the examination.
3.1.8 Performance evaluation
A panel member who fails to meet the IME performance standards reflects badly on the immigration medical program. Consequently, the panel member’s inclusion in the panel member network may be terminated. The performance of panel members is subject to regular evaluation and review.
Panel members should complete and provide, in a timely fashion, the required forms and documents requested by the RMO (e.g., panel member appointment forms, quality assurance activities, etc.). The procedure for completing the IME is discussed in Chapter 4 and is also subject to performance evaluation.
When requested by the RMO, panel members should make themselves and their staff available, within 7 days, for evaluation, monitoring, training, quality assurance, and/or educational activities and visits.
All complaints and disputes related to panel members’ performance in conducting IMEs will be evaluated (see Sections 3.4.9 and 3.4.10 for more information).
3.1.9 Absences from IME activities
- All anticipated absences from IME activities over 7 calendar days must be brought to the attention of the RMO and, where possible, an estimated date
of return to work should be provided to ensure that appropriate information is provided for the clients. - If the panel member will have a locum tenens replacing him or her during extended absences, the panel member must give the RMO at least 14 days’ notice, preferably by email. This will allow the RMO to activate the locum’s P number allowing him or her to use eMedical. Section 3.1.10 provides additional information on locum tenens.
- Panel members cannot submit IMEs if their leave information indicates that they are on leave.
- Extended or repeated unapproved absences may result in termination of a panel member’s status.
- After notification of the absence to the RMO:
eMedical-enabled Panel Clinics
- They are required to keep their contact information updated in the system.
- For personal and program integrity, they must enter leave dates directly in their personal record.
Paper-based Panel Clinics
- The RMO will update the information in their record in order to track the leave in their system.
3.1.10 Locum tenens
- Panel members who are planning to have persons replace them while they are away or assist them during high volume periods may request a locum tenens as follows:
- Contact the RMO to obtain medical officer approval;
- Submit the proposed substitute physician’s name and contact information, current resumé and a copy of the substitute physician’s medical registration/licence; and
- A statement from the proposed locum indicating that he or she has read this Handbook and agrees with the standards and requirements defined herein.
Note: Prior to recommending a particular physician or radiologist as a prospective locum, the panel member must be satisfied that the proposed locum has the qualifications and experience to perform IMEs.
- If the RMO approves the request, a written response (by letter or email) will be sent to the panel member. The panel member will then notify the locum that he or she has been authorized to provide services.
- The panel member must give the RMO at least 14 days’ notice, preferably by email, for every period of time where the locum will be acting on behalf of the panel member. This will allow the RMO to activate the locum’s P number allowing him/her to use eMedical.
- Panel members must ensure that the locum has adequate training in IME requirements, reporting procedures and any updates.
- CIC will provide the locum with a unique identifier (refer to Section 3.2).
- The termination of a panel member will automatically cancel prior approvals of a locum for this panel member.
eMedical-enabled Panel Clinics
- The locum will have his/her own password because the panel member’s password should not be shared. The system will be updated with appropriate information for locums.
Paper-based Panel Clinics
- The locum must sign the Medical Report (IMM 1017) “for and on behalf for Dr. ,” and use his or her personal wet stamp as required in Section 3.2.2 below.
3.1.11 Official languages
- English and French are the official languages of Canada and panel members must be able to communicate with Canadian officials in at least one official language.
- Panel members should inform CIC of the official language they prefer to use in correspondence.
- Panel members should inform CIC of the official language and any other language they speak. The IME must be completed in the Canadian official language requested by the client.
For eMedical users:
- Panel members must select either English or French prior to processing an IME in eMedical.
- Panel members should also indicate in the drop-down list in eMedical other languages they speak.
3.1.12 Use of interpreters
- When performing IMEs, panel physicians may examine clients who speak neither of the two official languages, nor any other language that the panel physician speaks. In these cases, an interpreter will be required.
- If an interpreter is used, panel members must select and ensure that the interpreter is unbiased and has no connection to the client. Family members or friends cannot act as an interpreter for a client. The use of a professional interpreter is at the client’s expense.
3.2 Unique identifiers for panel members
All panel members are given unique identifiers. These identifiers allow CIC to perform quality assessments of their work.
The unique identifier starts with the letter “P” followed by 8 or more digits (e.g., P12345678). This unique identifier will replace the designated medical practitioner stamp that was previously used. The panel member’s unique identifier will be embedded electronically in each IME or chest x-ray they submit through eMedical. For paper-based IMEs, the unique identifier must be clearly readable on each Medical Report (IMM 1017) and on each chest x-ray completed by a panel member (refer to Section 3.2.2 for additional information).
The panel member’s unique identifier should be included in all correspondence with CIC.
3.2.1 eMedical user identification
All eMedical users will have a unique logon ID and password to access the system. For panel members, the eMedical logon information will be linked electronically to the panel member’s unique identifier. The eMedical logon ID must not be disclosed to any other person or used by any other person to submit IMEs or chest x-rays.
3.2.2 Paper-based IME user identification
- For panel members or their locum tenens performing a paper-based IME, the unique identifier, along with their name, must be clearly readable on each Medical Report (forms IMM 1017 and IMM 5419) and on each chest x-ray.
- The panel member or their locum tenens must secure a stamp that features his/her name, the P#, the city and the country and must use that stamp in all correspondence with CIC. For example:
Name:
P#:
City, Country: - The unique identifier is used to identify each IME. It must be used on the front page of the IMM 1017 form “Client Biodata and Summary,” as well as on the “Laboratory Requisition and Report” and “Chest X-Ray Requisition and Report” sections of the IMM 5419 form.
- Each photo attached to the Medical Report (IMM 1017) must be stamped to confirm the identity of the client. Make sure that each IME is stamped and signed properly. In cases where the IMEs are not properly stamped and/or signed, CIC will refuse them and return the IMEs to the panel physician’s office.
- Panel radiologists may embed this information on the chest x-ray along with other required information about the client.
3.3 Guidelines for records management
Forms, documents and results of investigations required for the completion of IMEs are the property of CIC.
Panel members who perform IME-related activities must follow the procedures below for copies and files as well as for original documents and information. When documents are sent by courier, panel physicians must ensure that the IME forms and results are sent in appropriate order (refer to Appendix V for instructions) and should retain shipment tracking numbers for six months.
Information collected during the IME is for immigration medical purposes only. It may not be used for other purposes, including research, clinical studies or investigations, without appropriate consent of the client and CIC. Consent requests from CIC should be directed to:
Director of Operations
Health Branch
Citizenship and Immigration Canada
219 Laurier Ave. West, 3rd floor
Ottawa, ON K1A 1L1
eMedical-enabled Panel Clinics
- Original documents and information related to an IME must be forwarded to the responsible RMO electronically. Panel physicians are encouraged to save a full copy or a summary of the IME for their own records (e.g., in PDF format) and print out a full copy or a summary of the IME to give to the client (or the client’s parent or guardian), if the client wants a copy, before submitting it to the RMO, unless it would be injurious to the client’s physical or mental health.
- The panel physician can access the IME for 365 days after submitting the case. The panel physician can print a copy of the IME by clicking the “PRINT SUMMARY” button located at the bottom of the Health Case details window.
Paper-based Panel Clinics
- Original documents and information related to an IME must be forwarded to the responsible RMO by regular mail or commercial courier and must never be given to the client for delivery to the RMO.
- Panel physicians are encouraged to give a copy of the IME to the client (or the client’s parent or guardian) unless it would be injurious to the client’s physical or mental health.
- Panel physicians are required to keep copies and records of files for at least 2 years and in compliance with their local regulatory and licensing requirements.
3.4 Administrative instructions
CIC has instructions to guide panel members in various situations. These instructions cover a number of topics, such as the following:
- Communicating with the RMO;
- Advertising;
- Answering a client’s questions about the IME and about the immigration process;
- Responding to media inquiries;
- Resolving technical questions about eMedical;
- Establishing fees for IMEs; and
- Handling client complaints about the IME process or other immigration matters.
3.4.1 Communication with the regional medical offices
Regular contact will be maintained between panel members and RMOs regarding both medical and administrative issues. RMOs are the points of contact for panel members to address inquiries, questions and comments about individual immigration medical cases, examinations and about the immigration medial program. RMOs will also periodically update their panel members on IME processes. Questions and information on specific cases should always include identification details, such as the IME, unique medical identifier (UMI) or unique client identifier (UCI) number along with the client’s date of birth. To avoid possible breaches of confidentiality, information requests should never identify a client by name.
Written correspondence, such as letters, faxes or email, is preferred, but the telephone can be used when necessary (see Appendix I for RMOs’ addresses and contact information).
3.4.2 Advertising
Panel members may wish to advertise their IME services by creating their own website or distributing printed material, in which case the following instructions apply:
- No Canadian flag may be associated with the clinic;
- No CIC insignia may be associated with the clinic;
- No summary of the information on the CIC website may be provided, although links to the website are allowed;
- No eMedical insignia or logo may be included in the panel clinic advertisement; and
- Information about IME fees, services included in the fees, clinic’s address and contact information may be included in the advertisement.
3.4.3 Issues not related to immigration medical activities
From time to time, panel members may be contacted by other Canadian government officials. These officials may be seeking information about local health conditions, medical resources for consular services or help with a personal medical condition. Such requests are not related to the immigration medical program and panel physicians may respond to these inquiries as they choose. Fees for such services are at the member’s discretion. If in doubt, panel members may contact an RMO for guidance.
3.4.4 Communication with the media
On occasion, the media may become interested in the IME of a particular individual and contact the panel member for information. Under no circumstances should a panel member provide the media with information about a particular case.
Panel members should never communicate confidential information they are privy to with respect to the immigration system or to individual clients.
Panel members should refer all requests for comment or information to the RMO.
3.4.5 Communication issues related to clients
Clients may have questions about the immigration process, particularly when CIC officials request additional medical information or investigations. However, panel members are not authorized to explain or justify such requests. They should simply explain that the request came from CIC, that the panel physician is only a contact person between CIC and the client, and that the client should contact his/ her visa office to obtain additional information.
Specific questions about the IME process could include the following:
- total amount of time that CIC requires to complete the medical assessment process;
- amount of time between completion of the IME and subsequent steps of the immigration process or the issuing of a visa;
- administrative or policy aspects of the program; and
- other immigration-related issues.
These questions should be addressed to the immigration or visa office responsible for the case. The panel member may refer the client to the list of immigration and visa offices.
The panel member should never direct clients to the RMO. RMOs will not have all the information required to reply to most types of enquiries.
The panel member should never direct clients to the eMedical help desk. Panel members should ensure that their staff are aware of these instructions.
3.4.6 Enquiries about completing an IME
If panel members have non-eMedical-related questions regarding IMEs, they may contact their RMO listed in Appendix I. The panel member should have key information available to assist RMO staff, including the following:
- client’s full name;
- Date of birth;
- IME number, UMI number, and/or UCI number; and
- specific details of the question.
3.4.7 General eMedical system enquiries
Panel members who have questions about eMedical should consult the eMedical System User Guides and Quick Reference Guides.
For contact information related to eMedical, refer to Appendix I.
3.4.8 Fees for IMEs
Clients are responsible for paying all fees and costs associated with their IME. These fees include the following:
- panel physician services;
- radiological and laboratory services;
- consultations with specialists;
- investigations and treatment (e.g., when referred for treatment of TB or syphilis); and
- costs related to the sending of medical documents to the RMO.
Panel members may also charge a reasonable fee for the following:
- Follow-up visits in the case of furtherances;
- providing copies of the IME to the client upon request; and
- missed appointments in accordance with local standards of practice.
Panel members should charge reasonable fees and post a fees list in the clinic. Fees will reflect local conditions and service charges. Consequently, the fees for IMEs may vary from country to country and even within a country. If a panel member is completing a paper-based IME that must be mailed to the RMO, he or she should discuss the method and cost of sending the documents with the client beforehand.
Panel members in Canada should refer to Chapter 5 for instructions regarding requirements and fees for refugee claimants under the Interim Federal Health Program (IFHP).
Questions regarding fees and charges should be directed to the panel member’s RMO.
3.4.9 Incidents, complaints and quality assurance concerns
Clear and transparent procedures for responding to complaints and resolving disputes improve client service and the integrity of the immigration medical program. This section explains how CIC will deal with incidents, complaints and quality assurance concerns.
Incidents occurring during the IME process
If, during an IME, a panel member has a disagreement with a client, or confusion arises or an event occurs that might compromise client service, panel members should report these incidents to the RMO.
The following are examples of incidents that should be reported:
- The client becomes angry, threatening or violent toward the panel member or staff;
- The client claims that the panel member is deliberately delaying the IME process or requesting unnecessary investigations for personal gain;
- The client refuses to undergo parts of the examination or investigation;
- The panel member or clinic staff become aware of attempts by the client to falsify certain aspects of the IME, or clinical or laboratory investigations;
- The panel member or clinic staff are asked to overlook or alter some aspects of the IME, or of clinical or laboratory investigations;
- The client threatens to complain about the IME service or the IME process itself; or
- The panel member feels that reporting a one of a kind situation may benefit the program or increase other panel members’ knowledge.
Reports to the RMO should include the date of the incident, the client’s IME, UMI or UCI number and a brief description of the incident.
Complaints
Complaints are common in any client service procedure. Complaints regarding the IME and related services may arise from clients or other persons outside CIC. In addition, CIC personnel may provide critical comments or notifications of errors, performance issues or situations of concern regarding the IME and related services. Affected panel members will receive a letter of concern from the RMO and be given an opportunity to reply to the complaint. In accordance with the principles of natural justice and procedural fairness, privacy rules will not be breached when sharing the content of the complaint.
CIC’s Health Branch will consider the opinions and viewpoints of panel members and of anyone submitting a complaint or critical comment.
Quality assurance concerns
Health Branch officers will occasionally visit panel members to ensure the quality of their work. If concerns are found, the panel members will be asked to address them in a timely manner.
3.4.10 Resolution process for complaints or performance issues
Failure to meet performance standards may result in termination of the panel member’s designation. The following are examples of situations where panel members or their clinic staff would be seen to be failing to meet performance standards:
- Unacceptable behaviour or demonstrated misconduct:
- unprofessional or unethical conduct or activities;
- illegal activities; and
- loss or suspension of medical licence.
- Continued failure to maintain an acceptable level of performance as set out in this Handbook or in accordance with written instructions from the RMO. This includes continued or repeated deficiencies after notification, in the following:
- timely and correct completion of IMEs (including errors or omissions in the medical history and physical examination of clients);
- appropriately providing requisite laboratory and clinical investigations and activities;
- gathering and management of medical information;
- timely transfer of information and communication with the CIC Health Branch; and
- following the instructions in this Handbook.
Resolution of issues
Minor incidents and/or performance deficiencies will be addressed by the RMO in a letter outlining the necessary remedial or corrective measures, which may include additional training.
For serious complaints, such as harassment, sexual misconduct or illegal activities, the RMO will suspend the panel member, issue a letter summarizing the facts that gave rise to the complaint and provide the panel member with an opportunity to reply. While the panel member’s designation is suspended, IME activities by the panel member cease until the panel member is notified that he or she has been reinstated by CIC.
Upon receipt of the panel member’s reply, the RMO will conduct an assessment. If the response is deemed satisfactory, the panel member will be informed of the decision and be reinstated with appropriate recommendations. If the response is unsatisfactory, the panel member’s designation will be terminated.
Termination
CIC retains complete authority over the management of the panel member network. The number of panel members required may change in response to the local demand for IMEs. Panel physicians who are terminated because of operational needs will be notified in writing by the RMO at least 30 days prior to any such change in the network.
However, if the panel member’s designation is terminated because of performance deficiencies or complaints, there is no transition period and the termination is effective as of the date of the notification letter sent by the RMO.
Retirement and resignation
Panel members may retire or request removal from the panel network at any time. Panel members should send written notification to the RMO, including the anticipated date on which activity will cease.
Request for reconsideration
Panel members may request a reconsideration of a termination letter. Panel members should submit their request for reconsideration in writing within 30 days of receipt of the termination letter to:
Director of Operations Health Branch, CIC Canadian Building
219 Laurier Ave., West
Ottawa, ON K1A 1L1
CIC will consider all requests for reconsideration and make every effort to provide panel members with a written reply within 30 days of the receipt of their request for reconsideration. This decision is final.
Chapter 4: Immigration Medical Examination (IME)
This chapter provides panel members with a step-by-step method for completing an IME and associated forms.
The IME consists of a medical history, physical examination, age-specific laboratory tests and age-specific chest x-ray.
Mandatory age-specific laboratory and radiologic tests include:
- Urinalysis – clients ≥ 5 years
- Chest x-ray (postero-anterior view) – clients ≥ 11 years
- Syphilis – clients ≥ 15 years
- HIV – clients ≥ 15 years
Note: Screening of clients below the ages indicated may also be required. Consult the IMEI’s for more information.
With the launch of eMedical, the IME will be conducted, where technologically feasible, in a Web-based computer program designed for the electronic recording, transmission, processing and temporary storage of the IME and its associated results.
Panel members performing IMEs in a region where eMedical has been implemented must use the system to complete and submit all IMEs. Designation as a panel member is dependent on the ability to use the eMedical system. Only in the event of a system outage should paper IMEs be used by eMedical-enabled panel members.
Differences between the paper process and the eMedical process have been pointed out throughout this document.
IME paper forms have been redesigned to ensure consistency between eMedical IMEs and paper-based IMEs.
4.1 Verification of identity
4.1.1 Client identity confirmation
Client photographs are essential for ensuring that there is no substitution at any time during the lifecycle of the IME and that the person who undergoes the IME is the same person who is applying for entry to Canada. Photographs must be attached and submitted with the IME whether the IME is completed in eMedical or on paper.
eMedical-enabled Panel Clinics
- A live digital photograph of the client is taken in the clinic and uploaded in eMedical.
- Photographs must meet CIC’s photographic specifications standards.
- The eMedical system will include the photograph on all requisitions and referrals (laboratory, radiology, specialists and others).
Paper-based Panel Clinics
- The client must provide four photographs to the panel clinic.
- Photographs must meet CIC’s photographic specifications standards.
- If the photographs do not meet the specifications, ask the client to provide new photographs before their IME can be completed.
- A photograph must be attached to the Medical Report (IMM 1017) and to the laboratory and radiology requisitions/report forms (IMM 5419).
- The photograph on the Medical Report (IMM 1017) must be stamped in the top right corner with the panel physician’s ID stamp.
4.1.2 Identity documents
The client must submit a passport or other identification document acceptable for the Canadian Immigration medical examination. All documents must be valid (not expired).
Approved identification documents include the following:
- Original passport or a copy of passport certified by a Canadian Visa Office
- National ID Card (an original Birth Certificate is an acceptable national ID document for minors under the age of consent only.)
- Driver’s licence (in Canada only)
- Refugee travel document
- Red Cross travel document
- UN laissez-passer
- Seaman’s Book
- Organization of American States travel document
- Refugee Protection Claimant Document
Important: To ensure the integrity of the IME process, the same identity document must be used for all components of the IME, including laboratory, radiology and specialist referrals. The panel physician must inform the client accordingly.
4.1.3 Identity concerns
If the client provides personal details that seem inconsistent with the information on the submitted identity documents, panel members must identify the concern in the eMedical system or on the IMM 1017 – Medical Report (Client Biodata and Summary) for paper-based IMEs. A copy of the identity document of concern should be attached to the IME.
Panel members should complete the IME according to customary procedures. CIC will investigate the concern about the client’s identity.
eMedical-enabled Panel Clinics
- The identification document must be scanned and attached to the health case. The document will be submitted to CIC once the IME is completed.
Paper-based Panel Clinics
- Photocopies of the identification document concerned must be attached to the IME and submitted to CIC.
4.2 Client Consent and Declaration (IMM 5743)
See sample Client Consent and Declaration form in Appendix II.
Completion of the Client Consent and Declaration form is mandatory for all clients. If the client is under 16 years of age or is unable to provide consent (because of reduced mental capacity, for example), a parent or guardian may provide consent on his/her behalf.
eMedical-enabled Panel Clinics
The eMedical Client Consent and Declaration form includes the following:
- Declaration that all information provided during the IME is true, correct and complete;
- Declaration understanding that the IME information will be collected and temporarily stored on segregated databases located in Australia; and
- Consent for the collection and release of IME information related to the administration of Canada’s IRPA or to the protection of the health and safety of Canadians.
Paper-based Panel Clinics
The Client Consent and Declaration form for paper-based IMEs include the following:
- Declaration that all information provided during the IME is true, correct and complete; and
- Consent for the collection and release of IME information related to the administration of Canada’s IRPA or to the protection of the health and safety of Canadians.
If a client does not give consent, the IME cannot be carried out and the panel physician must notify the responsible RMO.
eMedical-enabled Panel Clinics
- eMedical will enter the client information on the Consent and Declaration form beforehand.
- The form should be printed from eMedical and provided to the client.
- Clinic staff or a panel member should review the Consent and Declaration form with the client and answer any questions.
- The client (or parent/guardian) must sign and date the document.
- The form must be scanned and uploaded to eMedical.
- Consent and Declaration check box must be ticked
- The IME cannot be submitted without the Client Consent and Declaration form appended.
Paper-based Panel Clinics
- Clinic staff must print and provide the form to the client.
- Clinic staff or a panel member should review the Consent and Declaration form with the client and answer any questions.
- The client (or parent/guardian) must sign and date the document.
- Clinic staff must attach the form and submit it along with the IME.
- The IME must not be submitted to the RMO without a completed Consent and Declaration form.
4.3 Medical Report: Client Biodata and Summary (IMM 1017)
See sample IMM 1017 form in Appendix III.
CIC has implemented one standard form, the Medical Report: Client Biodata and Summary (IMM 1017), for all immigration categories. This form displays the following:
- Client information (biodata);
- Immigration information;
- IMM Type: Excessive Demand Exempt (EDE); Non-EDE; refugee overseas
- IME grading; and
- Panel physician declaration.
The Medical Report (IMM 1017) issued by CIC includes information on the type of immigration category (IMM Type):
- EDE;
- Non-EDE; and
- Refugee overseas.
EDE
EDE clients are those who are exempted from assessment of excessive demand on the Canadian health care system.
However, EDE clients are assessed for:
- Danger to public health;
- Danger to public safety.
Non-EDE
Non-EDE clients are assessed for:
- Danger to public health;
- Danger to public safety;
- Excessive demand on the Canadian health care system.
Refugee overseas
Refugee overseas clients are also EDE.
Note: Panel physicians must complete and submit, either electronically or on paper, the IMM 5544 Resettlement Needs Assessment Form. See sample form in Appendix III.
Note: EDE clients include refugees, refugee claimants and certain family classes and individuals with protected person status.
The Medical Report (IMM 1017) form is typically issued by CIC with the client information and immigration information sections completed.
Clients who have been issued a Medical Report (IMM 1017) must present the form to the panel clinic when presenting themselves for their IMEs. The form will include two client identifiers: IME number and UCI number. (Note: This form may not include a client photo).
eMedical-enabled Panel Clinics
- Clinic staff will search for the client health case in eMedical using the IME# (search may also be done using client name and passport number, or UCI# or UMI#).
- Clinic staff should confirm the client’s identification by comparing the client’s information with the approved identification document (see Section 4.1.2).
- A live photo of the client is taken and uploaded to eMedical to verify identity throughout the life cycle of the IME.
- The IME and all of its components are then completed in the eMedical system
Paper-based Panel Clinics
- Clinic staff should confirm client’s identification by comparing the client’s information with the approved identification document (see Section 4.1.2).
- Clinic staff must attach a client photo (provided by the client) to the Medical Report (IMM 1017).
- The Medical Report (IMM 1017) will be completed and submitted along with all other IME forms.
4.3.1 Resettlement Needs Assessment (IMM 5544)
Clients who are being processed as refugees overseas will have a Resettlement Needs Assessment (IMM 5544) form issued to them along with their IMM 1017 by a Visa Office (VO). The form is available electronically in eMedical. Panel physicians must complete this form for all clients in the refugee overseas category.
Refer to the IMEI on the Resettlement Needs Assessment (IMM 5544) for detailed instructions on completing the form.
eMedical-enabled Panel Clinics
- VO issues IMM 1017 with IMM category of refugee overseas.
- IMM 5544 is included in medical instructions sent to client by VO as part of the IME.
- IMM 5544 will be automatically attached to the immigration medical examination in eMedical
- Submission of IME will include IMM 5544.
Paper-based Panel Clinics
- VO issues IMM 1017 with IMM category of refugee overseas.
- IMM 5544 is included in medical instructions sent to client by VO as part of the IME.
- Panel physician will complete the IMM 5544 along with the IME and submit them.
4.3.2 Upfront Medical (IMM 1017B Upfront)
UFM examinations are performed when clients report to a panel physician for their IME before a visa application has been submitted to CIC. Clients who are eligible for UFM examinations will not have a Medical Report (IMM 1017) issued by CIC nor will they have an existing file in the eMedical system.
Panel physicians should not refuse to examine these clients.
Panel physicians must ensure that they provide the client with the proof of having completed their upfront medical examination. For eMedical, the proof is the “Information Sheet” letter that they will print. For paper-based upfront medicals, it is the top page of the IMM 1017B Upfront form. Clients must include this proof when submitting their visa application.
Since an IME is valid for 12 months, panel physicians should remind clients to submit their visa application along with the proof of having completed their upfront medical examination well before the expiration of the 12 months; otherwise, the client may have to undergo a second IME.
eMedical-enabled Panel Clinics
- Panel physicians must first search eMedical for the client by their name and identity document number (e.g., passport number) to confirm that the client does not already exist in the system.
- If the client does not exist in eMedical, click “create case.”
- Enter the Client personal details (mandatory fields include Title, Family name, Gender, Date of birth and Country of birth).
- Enter the Identity Document Details. Clinic staff will check identity with the approved identification document. (Note: a live photo of the client must be taken and uploaded to eMedical at a later step during the IME.)
- Enter the Client’s Preferred Language.
- In the “Proposed Visa Application Details” section, select the appropriate upfront category from the drop down list (student, worker, visitor or family EDE). Note: For refugee claimants in Canada, select the category family EDE, and scan and attach the document provided by the client.
- Click “Create.”
- Proceed to upload and attach client photograph.
- Complete Identity Confirmation.
- An “Information Sheet” letter will be system generated and must be printed and given to the client for submission to CIC along with the visa application.
Paper-based Panel Clinics
- Panel physicians will use IMM 1017B Upfront paper forms, which have been provided to them and that are pre- populated with a UMI# and a barcode (see sample form in Appendix III).
- Clinic staff will check identity with a valid government-issued ID.
- Clinic staff must attach a client photo (provided by the client) to the form.
- Clinic staff must select the immigration category by checking the appropriate box (student, worker, visitor, family EDE or refugee claimant (in Canada only)).
- Page 1 of the IMM 1017B Upfront form “Copy to Client” must be completed and provided to the client for submission to CIC along with the visa application.
- Page 2 of the IMM 1017B Upfront form “Copy to Health Branch” must be completed and submitted to the RMO along with all other IME forms (e.g., IMM 5419, chest x-rays, lab results, etc.).
Note: It is very important to ensure the correct page goes to the client and the correct page goes to your RMO.
Page 1 — Client
Page 2 — RMO
4.4 IME grading
Prior to submitting the IME, the panel physician must provide a grade for the IME.
eMedical-enabled Panel Clinics
- An IME grade will be provided automatically by the system based on the reported findings.
- Grade A indicates that there are no abnormal findings present and no significant abnormal history.
- Grade B indicates that there are significant abnormal findings present and/or an abnormal history.
- If the system has provided an A-grade and the panel member believes that there are significant abnormal findings, he/she may change the grade to B.
- If the system has provided a B-grade, it cannot be changed to an A-grade.
- No comments are permitted for A-grade IMEs.
- Comments are mandatory for B-grade IMEs.
Paper-based Panel Clinics
- Panel members must provide an IME grade based on the reported findings.
- Grade A indicates that there are no abnormal findings present and no significant abnormal history.
- Grade B indicates that there are significant abnormal findings present and/or an abnormal history.
- Comments should not be included for A-grade IMEs.
- Comments are mandatory for B-grade IMEs.
4.5 Panel physician declaration
The panel physician declaration confirms the following:
- The client’s identity has been verified; and
- The IME and Medical Report are an accurate record of their findings.
eMedical-enabled Panel Clinics
- Panel physician’s declaration is provided electronically.
Paper-based Panel Clinics
- Panel physician’s declaration is provided in writing on the Medical Report (IMM 1017) and includes the panel physician’s name, signature, number and the date of the IME submission.
4.6 Medical History (IMM 5419)
See sample IMM 5419 form in Appendix III.
The panel physician uses the medical history to assess the client’s health. The medical history may be completed by the client or the clinic staff. If the client or clinic staff completes it, the panel physician must review and confirm the information provided.
Panel physicians must provide details with all “Yes” answers to medical history questions. CIC requires the following information:
- date of diagnosis;
- date of treatment or surgery;
- relevant medications; and
- current status of the condition (and, if applicable, the prognosis).
Panel physicians must provide this information in the comments section or they may attach a report to the IME.
The following table lists additional requirements when the answers to medical history questions show abnormality, whether the IME is completed in eMedical or on paper. Refer to the IMEIs for additional details.
| Medical History Questions | Related IMEI | IMM type | Requirements if abnormal |
|---|---|---|---|
| Tuberculosis (TB), treatment for tuberculosis | TB IMEI | EDE and non-EDE clients |
Chest x-ray (CXR), HIV, Hepatitis B and C, regardless of age |
| Close household or work contact with tuberculosis | TB IMEI | EDE and non-EDE clients |
TST and then CXR if TST is positive regardless of age (if CXR not already done) |
| Prolonged medical treatment and/or repeated hospitalization for any reason, including a major operation or mental illness | EDE and non-EDE clients |
Medical report | |
| Psychological/psychiatric disorder (including major depression, bipolar disorder or schizophrenia) | Psychiatric Conditions IMEI | EDE and non-EDE clients |
Psychiatrist's report |
| History of HIV | HIV IMEI | EDE and non-EDE clients |
HIV, CXR, Hepatitis B and C, syphilis, regardless of age, and HIV specialist report including CD4 count, HIV viral load, and when antiretroviral medications will be needed |
| An abnormal hepatitis B or C blood test | Hepatitis / Liver Disease IMEI |
EDE and non-EDE clients |
HIV, CXR, Hepatitis B and C, syphilis, regardless of age |
| Cancer or malignancy in the last five years | Cancer IMEI | EDE and non-EDE clients |
Oncology report |
| Diabetes | Diabetes IMEI | EDE and non-EDE clients |
Screen for signs or symptoms and presence of end-organ damage. Urinalysis, serum creatinine (eGFR if abnormal) and HbA1c; regardless of age |
| Heart condition including coronary disease, hypertension, valve or congenital disease | Cardiac Disease IMEI and Hypertension IMEI | EDE and non-EDE clients |
Screen for signs or symptoms (including blood pressure) and presence of end-organ damage. Serum creatinine, regardless of age |
| Blood condition (including thalassemia) | EDE and non-EDE clients |
Check for history of admission | |
| Kidney or bladder disease | Renal disease IMEI |
EDE and non-EDE clients |
Urinalysis, serum creatinine (eGFR if abnormal) regardless of age |
| An ongoing physical or intellectual disability affecting your current or future ability to function independently or be able to work full-time (including autism or developmental delay) | Psychiatric Conditions IMEI and Cognitive Impairment IMEI | EDE and non-EDE clients |
Activities of daily living (ADL), Global assessment of functioning (GAF), Chart of Early Childhood Development (CECD) and/or an assessment of cognitive functioning |
| Addiction to drugs or alcohol | Psychiatric Conditions IMEI | EDE and non-EDE clients |
Psychiatrist’s report and if evidence of IV drug use, HIV, Hepatitis B and C, regardless of age |
| Prescribed pills or medication (excluding oral contraceptives, over- the-counter medication and natural supplements) | EDE and non-EDE clients | List relevant medications and mention the indication | |
| For female clients: a) Are you pregnant? |
EDE and non-EDE clients | ||
| b) If yes, what is the expected date of delivery? | Attach IMM 5733 Instructions for Pregnant Client − X-Ray Deferred for paper based IME’s. eMedical generates this Pregnancy Deferral Letter. | ||
| c) If yes, do you wish to defer your chest x-ray at this time? |
4.6.1 Pregnant client
If the client chooses to defer her CXR because of pregnancy:
eMedical-enabled Panel Clinics
- CIC is informed electronically by eMedical when a CXR is deferred and the health case is put on hold when a client is pregnant and chooses to defer her CXR;
- CXR requisition and instructions are generated by eMedical and provided to the client;
- eMedical generates a “Pregnancy deferral letter” with instructions for the client;
- All other components of the IME are completed and the IME is put on hold status until the CXR is completed;
- The IME will be submitted to CIC along with the CXR results when available.
Paper-based Panel Clinics
- The CXR requisition is completed by the panel physician and given to the client;
- The IMM 5733 Instructions for Pregnant Client Letter is completed by the panel physician and given to the client;
- The client may forward a copy of the IMM 5733 Instructions for Pregnant Client Letter to the visa office as proof that the IME has been started and that the CXR has been deferred because of pregnancy;
- The panel physician may complete the IME, except for the CXR; and
- The IME is only submitted once the post partum CXR is returned to the panel physician;
- See sample of the IMM 5733 Instructions for Pregnant Client − X-Ray Deferred form in Appendix III.
4.7 Physical Examination (IMM 5419)
See sample IMM 5419 form in Appendix III.
The physical examination must be completed by the panel physician.
Panel physicians must provide details of all abnormal findings during the physical examination. CIC requires the following information:
- history;
- diagnosis;
- treatment details (including dates and medications);
- lab results;
- specialist reports (as required);
- current status; and
- prognosis.
Panel physicians may enter this information in the comments section or attach a report to the IME.
The following table lists the additional requirements when the answers to physical examination questions show abnormality, whether the IME is completed in eMedical or on paper. Refer to the IMEIs for additional details.
| Physical Examination | Related IMEI | IMM type | Requirements if abnormal |
|---|---|---|---|
| Was a chaperone offered? | Breast Exam IMEI | EDE and non-EDE clients | |
| Height (cm) (all clients) | Percentile IMEI | EDE and non-EDE clients | HIV testing, specialist pediatrician and school reports (if applicable) |
| Height percentile (clients ≤ 2 years of age) | |||
| Weight (kg) (all clients) | Percentile IMEI | EDE and non-EDE clients | HIV testing, specialist pediatrician and school reports (if applicable) |
| Weight percentile (clients ≤ 2 years of age) | |||
| BMI (clients ≥ 18 years) | BMI IMEI | EDE and non-EDE clients | If underweight: refer to HIV IMEI If overweight: refer to IMEIs on cardiac disease, hypertension, diabetes, renal disease, serum creatinine and urinalysis |
| Head circumference (cm) (clients ≤ 2 years of age) | |||
| Head circumference percentile (clients ≤ 2 years of age) | Percentile IMEI | EDE and non-EDE clients | Specialist pediatrician and school reports (if applicable) |
| Ear/nose/throat/mouth | EDE and non-EDE clients | ||
| Hearing | Hearing impairment and deafness IMEI | EDE and non-EDE clients | Provide specialist report(s) |
| Eyes (including fundoscopy) | EDE and non-EDE clients | ||
| Best distance visual acuity (with or without correction) | EDE and non-EDE clients | ||
| Blood pressure (clients ≥ 15 years of age) Normal readings
|
Hypertension IMEI | EDE and non-EDE clients | Repeat blood pressure |
| Repeated blood pressure (clients ≥ 15 years of age) Normal readings
|
Hypertension IMEI | EDE and non-EDE clients | Screen for signs or symptoms (including blood pressure) and presence of end-organ damage serum creatinine regardless of age |
| Cardiovascular system | Cardiac disease IMEI | EDE and non-EDE clients | Serum creatinine regardless of age and cardiologist report when required |
| Respiratory system | TB IMEI | EDE and non-EDE clients | If signs of TB: CXR, HIV, Hepatitis B and C regardless of age |
| Nervous system: sequelae of stroke or cerebral palsy, other neurological disabilities | Debilitating conditions, ADL, GAF and/or CECD IMEIs | EDE and non-EDE clients | ADL, GAF, CECD and/or an assessment of cognitive functioning |
| Mental and cognitive state | Cognitive impairment, ADL, GAF and/or CECD IMEIs | EDE and non-EDE clients | ADL, GAF, CECD and/or an assessment of cognitive functioning |
| Intellectual ability | Cognitive impairment, ADL, GAF and/or CECD IMEIs | EDE and non-EDE clients | ADL, GAF, CECD and/or an assessment of cognitive functioning |
| Developmental milestones (clients ≤ 5 years of age) | CECD IMEI | EDE and non-EDE clients | CECD and pediatrician report (optional) |
| Gastrointestinal system | Hepatitis / Liver Disease IMEI | EDE and non-EDE clients | If hepatomegaly: Hepatitis B and C screening, and then ALT and specialist report if positive |
| Musculoskeletal system | Debilitating conditions IMEI and ADL IMEI | EDE and non-EDE clients | ADL regardless of age |
| Skin and lymph nodes | Cancer IMEI and HIV IMEI | EDE and non-EDE clients | Screen for skin cancer, leprosy, surgical scars, tattoos and piercings. Inspect neck, axilla and groin for lymphadenopathy |
| Evidence of substance abuse (e.g., venous puncture marks) |
Psychiatric Conditions IMEI | EDE and non-EDE clients | Psychiatrist’s report and if evidence of IV drug use HIV, Hepatitis B and C, regardless of age |
| Breast examination | Breast Exam IMEI | EDE and non-EDE clients | Investigate (e.g., ultrasound, mammogram, specialist report) |
| Endocrine system (such as evidence of complications from diabetes) | Diabetes IMEI | EDE and non-EDE clients | If diabetes, proceed with screening |
| Are there any physical or mental conditions that may prevent this person from attending a mainstream school, obtaining full-time employment or living independently now or in the future? | Psychiatric Conditions IMEI and Cognitive Impairment IMEI | EDE and non-EDE clients | ADL, GAF, CECD and/or an assessment of cognitive functioning |
4.8 Laboratory Requisition and Report
See sample Laboratory Requisition and Report (in form IMM 5419) in Appendix III.
eMedical-enabled Panel Clinics
- eMedical will generate laboratory requisitions with client biodata and photograph already printed on them.
- Mandatory tests will be system generated according to client’s age and clinical findings.
Paper-based Panel Clinics
- The Laboratory Requisition and Report should be completed with client’s personal information entered: surname, given name, date of birth, IME# or UMI# (if applicable).
- Client photograph must be attached to ensure IME integrity for laboratory testing.
- Indicate with a checkmark (R) the tests required.
Laboratory staff are required to confirm the client’s biodata/identity by comparing the photograph on the Laboratory Requisition and Report, the photograph on the client’s approved identity document and the client reporting for laboratory tests.
Any identity concerns must be documented either in eMedical or on the paper laboratory requisition forms. Laboratory testing may continue and the panel physician will report the concerns to CIC for follow-up.
Laboratory staff must fill out the declaration to confirm the following:
- The requested laboratory tests have been performed; and
- The sample for testing was collected from the client identified on the requisition.
4.8.1 Urinalysis
A urinalysis is mandatory for all clients five years of age or older.
Refer to the urinalysis IMEI for detailed recommendations on screening.
4.8.2 Syphilis serology
Syphilis is endemic in many regions of the world from which CIC clients originate i.e., South and Southeast Asia, sub-Saharan Africa, Latin America and the Caribbean.
Panel physician must pay special attention during IME for all clients that have risk factors for syphilis, particularly those originating from the regions of high incidence of syphilis mentioned above.
Syphilis testing is mandatory for all clients 15 years of age or older. Testing is also necessary for all clients below the age of 15 who have any of the following risk factors:
- signs and symptoms compatible with syphilis diagnosis;
- history of unprotected anal or vaginal sex or pregnancy;
- history of another sexually transmitted infection such as HIV, herpes, chlamydia, gonorrhoea or bacterial vaginosis; or
- history of being born to a syphilitic mother.
Refer to the syphilis IMEI for detailed recommendations on screening.
For confirmation purposes, a test should be repeated if the result is indeterminate. For positive syphilis serology results, panel physicians will:
- treat according to the Canadian Guidelines on Sexually Transmitted Infections and provide proof of treatment; or
- accept previous treatment carried out according to the Canadian Guidelines on Sexually Transmitted Infections and provide proof of treatment.
CIC requires the following treatment information:
- dates;
- medications; and
- dosages.
Proof of treatment information may either be included in the General Supporting comments of the syphilis test section or a report may be attached to the IME.
4.8.3 HIV serology
HIV screening is required for all clients 15 years of age or older undergoing an IME. Panel physicians must also request HIV screening for clients below the age of 15 who have any of the following risk factors:
- signs and symptoms compatible with HIV diagnosis;
- history of unprotected anal or vaginal sex or pregnancy;
- history of another sexually transmitted infection such as syphilis, herpes, chlamydia, gonorrhoea or bacterial vaginosis;
- history of sharing needles, syringes and other equipment and drug solutions for injecting drugs;
- history of receiving unsafe injections, blood product transfusions or medical procedures that involve unsterile cutting or piercing;
- accidental needle stick injuries, including among health workers;
- suspected active TB or hepatitis B or C;
- tattooing, piercing or having received acupuncture;
- history of being born to an HIV positive mother; or
- any child showing failure to thrive.
Refer to the HIV IMEI for detailed recommendations on screening and pre- and post-test counselling.
All HIV positive results must be confirmed with a Western blot test or a second ELISA from a different manufacturer. Panel physician must provide post-test counselling to all HIV positive cases and must have the client sign the IMM 5728: Acknowledgment of HIV Post-Test Counselling form (see Appendix III).
HIV specialist reports including CD4 and Viral Load are required for all HIV positive clients.
4.9 Chest X-Ray Requisition and Report
See Chest X-Ray Requisition and Report (in form IMM 5419) in Appendix III.
Routine postero-anterior chest x-rays are mandatory for clients 11 years of age or older. A panel physician should request a chest x-ray, regardless of age, if the medical questionnaire reveals a past history of TB infection or treatment in the client or his/her close contacts.
Chest x-rays must be examined for general radiological findings and, more specifically, for evidence of active or inactive TB disease.
Radiology clinic staff are required to confirm client identity and biodata by comparing the photograph on the radiology requisition and report, the photograph in the eMedical system (for eMedical-enabled panel clinics), the photograph on the client’s approved identity document and the client reporting for chest x-rays.
Any identity concerns must be documented either in eMedical or on paper forms. The panel radiologist may continue with the chest x-ray and the panel physician will report the concerns to CIC for follow up.
The chest x-ray must contain the following information:
- client’s name;
- client’s date of birth;
- client’s gender; and
- date of the chest x-ray.
eMedical-enabled Panel Clinics
- Clients must bring their IME#, UMI#, UCI# with them in order to undergo their chest x-ray; and
- Panel radiology clinic staff will use the IME#, UCI#, UMI# or the client’s name and passport # to retrieve the client’s health case in eMedical.
Paper-based Panel Clinics
- Panel physician must enter the client’s personal information on the chest x-ray requisition form: surname, given name, date of birth, IME# or UMI# (if applicable); and
- The client’s photograph must be attached to the radiology requisition.
There may be cases where a client may not be pregnant at the time of the IME, but is pregnant at the time of the x-ray examination. If a client is pregnant and elects to proceed with the chest x-ray examination, there are no changes to the chest x-ray procedures.
If the client chooses to defer her chest x-ray because of pregnancy:
eMedical-enabled Panel Clinics
- CIC is informed electronically by eMedical that the client is pregnant along with her estimated date of delivery;
- eMedical generates a “Pregnancy deferral letter” with instructions for the client;
- The IME is put on hold status until the chest x-ray is completed; and
- The IME will be submitted to CIC along with the CXR results when available.
Paper-based Panel Clinics
- The radiology clinic must notify the panel physician that the chest x-ray has been deferred;
- The panel physician may complete the IME, except for the chest x-ray; and
- The IME is only submitted once the post partum chest x-ray is returned to the panel physician.
- See sample of the IMM 5733 Instructions for Pregnant Client − X-Ray Deferred form in Appendix III.
4.9.1 Chest x-rays indicating active tuberculosis
eMedical-enabled Panel Clinics
- Panel radiologist’s indication of suspected active TB in the client’s chest x-ray will generate an Active TB warning flag for the panel physician.
- Panel physicians must arrange for immediate referral for TB investigation.
- For all confirmed active TB cases, panel physicians must notify their public health authorities according to the country’s or region’s public health guidelines and directives as well as ensure that treatment provided follows WHO recommendations and protocols (http://whqlibdoc.who.int/publications/2010/9789241547833_eng.pdf ).
- Panel physicians can now submit the health case in eMedical.
- For all confirmed active pulmonary TB cases, panel physicians must conduct screening for hepatitis B and C, as well as HIV (if not already done), and proceed with contact screening for all family members or close contacts who are also CIC clients. Treatment for latent TB should be recommended for contacts as per instructions. If health case has been submitted this screening will be requested as a furtherance process by the RMO.
- Refer to the TB IMEI for more information.
Paper-based Panel Clinics
- A panel radiologist who indicates suspected active TB in the client’s chest x-ray must notify the panel physician immediately.
- The chest x-ray and report are sent to the panel physician for submission to CIC along with the panel physician’s examination results.
- Panel physicians must arrange for immediate referral for TB investigation.
- For all cases of active TB, panel physicians must notify their public health authorities according to the country’s or region’s public health guidelines and directives as well as ensure that treatment provided follows WHO recommendations and protocols (http://whqlibdoc.who.int/publications/2010/9789241547833_eng.pdf ).
- For all confirmed active pulmonary TB cases, panel physicians must conduct screening for hepatitis B and C, as well as HIV (if not already done), and proceed with contact- screening for all family members or close contacts who are also CIC clients. Treatment for latent TB should be recommended for contacts as per instructions.
- Refer to the TB IMEI for more information.
- Panel physicians must complete the IME and submit it to CIC.
4.9.2 Radiology grading
Prior to submitting the chest x-ray, the panel radiologist must provide a grade for the radiography.
eMedical-enabled Panel Clinics
- A radiology grade will be provided automatically by the system based on the reported findings.
- Grade A indicates that there is no evidence of active TB or changes suggestive of other significant diseases identified.
- Grade B indicates that there is evidence of active TB or changes suggestive of other significant diseases identified.
- If the system has provided an A-grade and the panel radiologist believes that there is evidence of active TB or changes suggestive of other significant diseases, he/she may change the grade to B.
- If the system has provided a B-grade, it cannot be changed to an A-grade.
- No comments are permitted for A-grade chest x-rays.
- Comments are mandatory for B-grade chest x-rays.
Paper-based Panel Clinics
- Panel radiologists must provide a radiology grade based on the reported findings.
- Grade A indicates that there is no evidence of active TB or changes suggestive of other significant diseases identified.
- Grade B indicates that there is evidence of active TB or changes suggestive of other significant diseases identified.
- Comments should not be included for A-grade chest x-rays.
- Comments are mandatory for B-grade chest x-rays.
4.9.3 Panel radiologist declaration
The panel radiologist declaration confirms the following:
- The client’s identity has been verified; and
- The radiology report is an accurate record of the radiologist’s findings.
eMedical-enabled Panel Clinics
- Panel radiologist declarations are provided electronically.
- Radiology Support can declare on behalf of a panel radiologist
Paper-based Panel Clinics
- Panel radiologist declarations are provided in writing on the radiology report and include the panel radiologist’s name, signature, number and the date of the chest x-ray report.
4.9.4 Submission of chest x-rays
eMedical-enabled Panel Clinics
- Digital chest x-rays are uploaded to the eMedical system.
- The panel radiologist or authorized radiology support staff enter the general and special findings in the eMedical system.
- The chest x-ray is graded in the eMedical system and submitted to the client’s IME.
- The panel physician clinic is notified of the completion of the chest x-ray examination.
- The panel physician reviews the radiologist report and grading.
- Once all examinations are completed, the IME will be submitted to CIC by the panel physician.
Paper-based Panel Clinics
- The panel radiologist provides the general and special findings and grades the digital chest x-rays or film using the proper form.
- The panel radiologist or authorized radiology staff forward the chest x-rays and the report to the panel physician.
- The panel physician reviews the radiologist’s report and grading.
- Once all examinations are completed, the IME is sent to CIC by the panel physician.
4.10 Furtherance process
RMOs may require additional information to complete the medical assessment. This additional information is obtained through the furtherance process. Additional cost to the client may occur if e.g the initial IME was not done by the panel physician involved in the furtherance.
Panel physicians are responsible for the following:
- Referring the client for additional testing or to an appropriate specialist for consultation (see sample IMM 5734 Specialist’s Referral Form in Appendix III);
- Selecting the specialist (the client may not select his/her own specialist, although the client’s previous medical records may be provided along with the additional requested reports); and
- Completing the furtherance requirements and submitting results to the RMO.
eMedical-enabled Panel Clinics
- The RMO issues a client letter with instructions to return to a panel physician for further investigations.
- The furtherance request is transferred to eMedical.
- The panel physician retrieves the furtherance request from eMedical by carrying out a search using the IME# or UCI# indicated in the client’s letter.
- The panel physician completes the additional examination(s) or generates a referral letter containing the information that will be sent to a specialist for the required investigation(s).
- The panel physician enters the information in eMedical and submits the information to CIC.
Paper-based Panel Clinics
- The RMO issues a client letter with instructions to return to the panel physician and also provides the client with a sealed letter for the panel physician along with detailed instructions for further investigations.
- NOTE: IF a furtherance is issued on paper it cannot be completed in eMedical.
- The panel physician completes the additional examination(s) or refers the client to a specialist for the required investigation(s).
- The referral letter must include the client’s biodata and photograph and clearly indicate the required investigations requested by CIC.
- Once all the required investigations have been completed, the panel physician returns the reports to CIC.
4.11 Additional forms and information
See Appendix III for samples of the following additional forms:
- IMM 5725: Activities of Daily Living (ADL)
- IMM 5727: Global Assessment of Functioning (GAF)
- IMM 5738: Chart of Early Childhood Development (CECD)
Chapter 5: Panel Members’ Activities in Canada
This chapter of the Handbook provides information, instruction and reference material for panel members operating in Canada. It does not apply to panel members who perform Canadian IMEs in other countries.
5.1 Providing primary care for IME clients
If the panel physician is asked to become the personal physician of an immigration client, he or she should make sure that the client understands the different duties and responsibilities of panel physicians and personal physicians. It must also be understood that any medical services not related to the IME or covered under the IFHP will not involve CIC.
5.2 Providing services in Canada’s official languages
In Canada, CIC is committed to providing clients with the opportunity to receive their IME in their preferred official language, either English or French. If a panel physician is unable to provide service in the preferred official language of the client, he/ she should refer the client to the nearest panel physician who can. If there is no panel physician nearby who is able to do so, the panel physician should advise the client or his/her representative to contact the CIC Call Centre at 1-888-242-2100 for more information.
5.3 Protection of personal information
In addition to the Privacy Act, the Access to Information Act, the Canadian Charter of Rights and Freedoms and the Library and Archives Act, personal information in Canada is protected under the Personal Information Protection and Electronic Documents Act (PIPEDA) and under provincial and territorial privacy legislation. The laws of other jurisdictions where the information is collected may also apply. Panel physicians must
comply with these laws when collecting information because the laws set out principles for the collection, use, disclosure, retention and disposal of personal information.
In order to comply with legislation, the IME forms, in some instances, require clients to consent to the disclosure of their personal health information to third parties. In addition, personal health information must be collected and stored in such a way that it is protected from unauthorized disclosure. Panel physicians in Canada receive advice from their professional organizations or regulating bodies on how the PIPEDA and provincial or territorial privacy legislation are to be applied, as well as on the steps required to properly manage information. The PIPEDA can be viewed at http://laws.justice.gc.ca/en/P-8.6/.
5.4 Refugee determination system in Canada
Refugee claimants (often referred to as asylum seekers) are individuals who, following their arrival in Canada, make a formal claim to a CIC or Canada Border Services Agency officer requesting Canada’s protection.
Under the IRPA, all persons claiming refugee protection must undergo an IME. The IME forms and requirements for this refugee group are the same as for other immigrants.
As stated earlier in this Handbook, immigrants are examined in order to identify medical conditions that might affect their admissibility to Canada under the IRPA (see Section 2.1). Refugee claimants are EDE. This means that they are examined primarily to identify conditions that might pose risks to public health and public safety; however, any additional services required by the IMEIs may also be provided.
Refugee claimants are referred for their IME when they file their claims. They are given medical instructions and a list of panel physicians. They must undergo their IME within 30 days following their claim for refugee status.
Refugee claimants who have been granted protected person status by the Canadian authorities become eligible to apply for provincial or territorial health insurance. They must undergo a second IME as part of their application for permanent residence.
They are also given medical instructions and a list of panel physicians. The medical examination is to be undertaken within 90 days of issuance of the IME form IMM 1017.
5.5 Interim Federal Health Program (IFHP)
Refugee claimants may be eligible to have some of their health costs covered under the IFHP. This program, funded by CIC, provides limited, temporary coverage of costs related to health care for specific categories of people, including protected persons, refugee claimants, rejected refugee claimants, certain persons detained under the IRPA and other specified groups. Adjudication and payment of claims for the program is provided by the IFHP Claims Administrator, Medavie Blue Cross.
A panel member and any other providers assisting with IME-related tests must register as an IFHP Provider with Medavie Blue Cross, comply with the provider’s terms and conditions, and follow all procedures for clients eligible under this program.
With the reform of the IFHP, effective on June 30, 2012, the following changes were applicable:
- The IFHP does not cover the cost of IMEs for protected persons. Other paid medical IME and related tests for individuals determined to be protected persons by the IRB are no longer covered under the IFHP. Protected persons are responsible for paying for the costs of their IME.
- The IFHP will continue to cover the cost of IMEs and related tests for refugee claimants.
- The IFHP will not cover IMEs or related tests for rejected refugee claimants.
For more information on the IFHP, visit cic.gc.ca/ifhp.
As a general rule, only panel physicians are authorized to perform IMEs for IFHP beneficiaries. In certain cases, CIC may approve a non-panel physician. It is important to note that unless authorized by CIC to perform IMEs, Medavie Blue Cross will not reimburse non-panel physicians for this service and the examination documents will not be accepted by CIC as an IME.
Important Information
Verifying IFHP eligibility
- Panel physicians must check with Medavie Blue Cross that their patient’s IFHP coverage is still current BEFORE the examination is carried out because client eligibility may be cancelled or modified without notice should their immigration status change. For example, if a beneficiary receives IFHP coverage as a detainee, once released from detention, their IFHP detainee coverage is terminated. They must then reapply to CIC to have their previous IFHP coverage reinstated in order to continue to be covered under the program. Please also note that because of normal delays between the production and uploading of the files, it can take 2 working days for an IFHP beneficiary’s coverage to become active in Medavie Blue Cross’ system.
Panel physicians cannot refuse to provide IMEs for persons covered by the IFHP but may charge for missed appointments in accordance with local standards of practice. This charge will not be reimbursed under the IFHP.
Coding benefits
- CIC determines the fees for IMEs and related tests when reimbursed under the IFHP. The current IFHP codes and fees can be found in the IFHP Benefit Grid – IME and IME Tests at https://provider.medavie.bluecross.ca under section Benefit Grid/Drug Formulary.
- Panel physicians submitting claims for IMEs and related tests must use the appropriate benefit codes listed in the IME Benefit Grid.
Billing for services
- Invoices for services listed in the IME Benefit Grid must be sent to Medavie Blue Cross.
- Panel physicians must not ask patients who are eligible for IFHP IME coverage to pay surcharges or additional costs, or ask for a deposit or any other fee in connection with the IME.
The IFHP provides coverage for more than the IME, as described in the IFHP Information Handbook for Health Care Professionals (Provider Handbook). Chapter 9 in the Provider Handbook contains important information for panel physicians who perform IMEs for refugee claimants.
The Provider Handbook, IFHP Benefit Grid and all other program information, including prior approval procedures, claim submission guidelines, provider terms and conditions as well as payment procedures can be found online at https://provider.medavie.bluecross.ca.
5.6 Public Health Liaison Unit
Note: The Public Health Liaison Unit (PHLU) was formerly known as the Medical Surveillance Unit (MSU).
Individuals who in the course of an IME are found to have inactive TB or treated syphilis must be placed under medical surveillance in Canada. The PHLU reports such cases to the appropriate provincial or territorial public health authorities.
Under the PHLU mandate, panel physicians in Canada are not released from their responsibility to notify provincial and territorial public health authorities of conditions and diseases that must be reported under the legislation of the province or territory in which they practise.
At no time should routine investigation or management of active or suspected active TB be deferred or delayed because of immigration medical activities. If a Canadian panel physician cannot contact a client suspected of having an active infectious disease, he or she should immediately inform the CIC Health Branch (see contact information in Appendix I).
Appendix I: Contact Information
In Canada
Operations Directorate
Mail: Director of Operations
Health Branch
Citizenship and Immigration Canada
219 Laurier Ave. West, 3rd floor
Ottawa, ON K1A 1L1
Interim Federal Health Program
Mail: Director, Interim Federal Health Program
Health Branch
Citizenship and Immigration Canada
219 Laurier Ave. West, 3rd floor
Ottawa, ON K1A 1L1
Email: IFH-PFSI@cic.gc.ca
IFHP Medavie Blue Cross
Mail: 644 Main St., P.O. Box 6000
Moncton, NB E1C 0P9
Provider website: https://provider.medavie.bluecross.ca
Customer Service Centre: 1-888-614-1880
Email: CIC_Inquiry@medavie.bluecross.ca
Fax for inquiries: 506-867-4651
Panel Physician Program
Mail: Manager, Immigration Medical
Examination Program
Operations Directorate
Health Branch
Citizenship and Immigration Canada
219 Laurier Ave. West, 3rd floor
Ottawa, ON K1A 1L1
Email: PanelMember@cic.gc.ca
eMedical systems support
For system support
English speaking panel members
Contact DIAC via the panel physician web enquiry form
French speaking panel members
Contact CIC at the following:
Email: NHQ-eMedical-Mailbox@cic.gc.ca (available from 9:00 a.m. to 5:00 p.m., Canadian EST, Monday to Friday, excluding statutory holidays)
For critical incidents
Contact IT support immediately:
- Telephone: +61 2 6264 0400
- Email: itsupport@immi.gov.au
Critical incidents include the following:
- Total loss of the eMedical system(unexpected outages)
- Loss of core functions (cases cannot be submitted; attachments cannot be uploaded)
(Note: This service is provided by DIAC 24 hours a day, 7 days a week in English only.)
For enquiries regarding medical clinical issues
Panel members should continue to direct all IME-related enquiries to their RMO.
Regional Medical Offices
Beijing
Mail: Overseas Regional Medical Office
Canadian Embassy
19 Dongzhimenwai Dajie
Chaoyang District
Beijing, PRC 100600
Fax: +86 10 5139 4467
Email: Bejing-mc@international.gc.ca
London
Mail: Overseas Regional Medical Office High Commission of Canada MacDonald House
38 Grosvenor Street
London, UK W1K 4AA Fax: +44 (0) 20 7258
Email: London.pp@international.gc.ca
Manila
Mail: Overseas Regional Medical Office
Canadian Embassy
Level 7, Tower 2, RCBC Plaza
6819 Ayal Avenue, Makati City
0707, Philippines
Fax: +632 843 1103
Email: Manil.mc-im@international.gc.ca
Manil.mc@international.gc.ca
New Delhi
Mail: Overseas Regional Medical Office
High Commission of Canada
7/8 Shantipath, Chanakyapuri
New Delhi 110021, India
Fax: +91 11 41782020
Email: Delhi-mc@international.gc.ca
Americas
Mail: Ottawa Regional Medical Office
Health Branch
Citizenship and Immigration Canada
219 Laurier Ave. West, 3rd floor
Ottawa, ON Canada K1A 1L1
Fax: +1 613 954 6211
Email: NHQ-HB-DMP-Inquiries@cic.gc.ca
Paris
Mail: Overseas Regional Medical Office
Canadian Embassy
35 Montaigne Avenue
75008 Paris, France
Fax: +33 1 44 43 29 83
Email: Paris-mc@international.gc.ca
Appendix II: Client Consent and Declaration
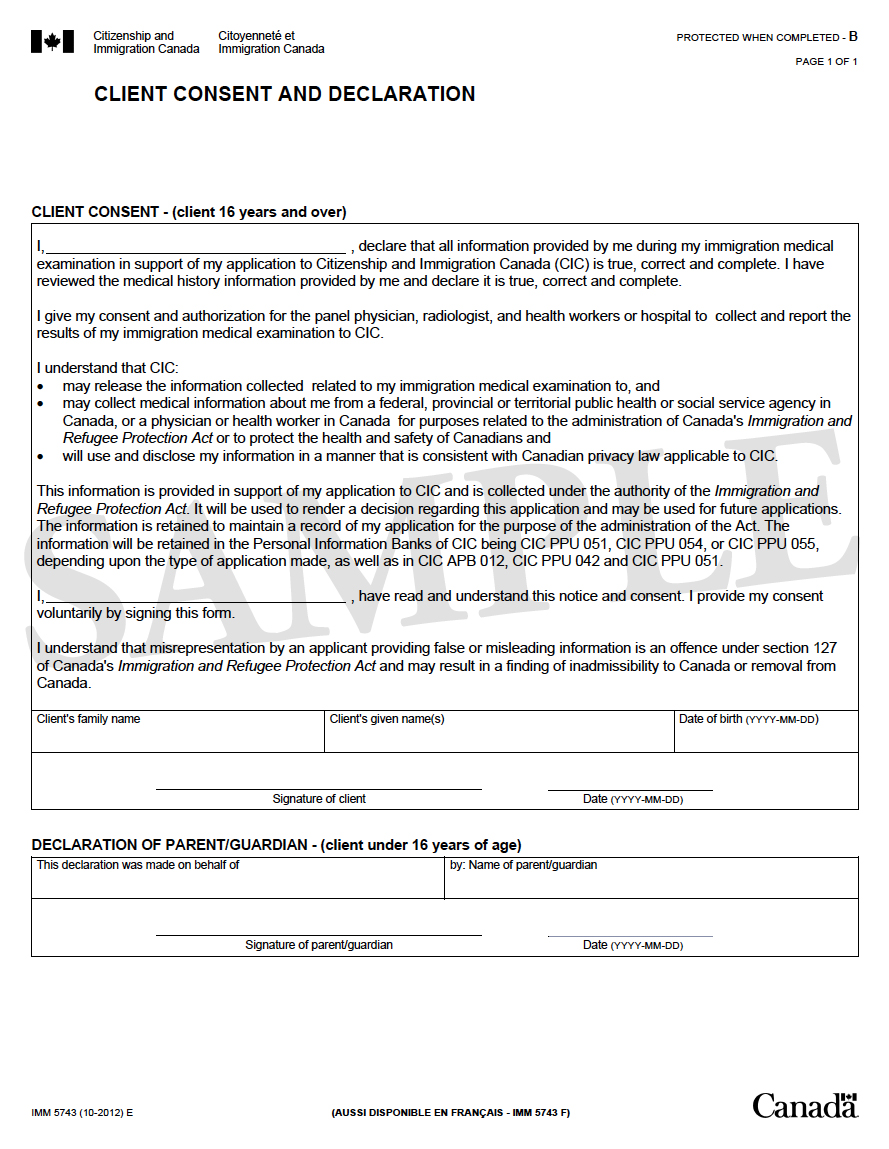
Appendix III: Forms
- IMM 1017: Medical Report – Client Biodata and Summary
- IMM 1017B Upfront: Upfront Medical Report – Client Biodata and Summary
- IMM 5419: Medical Report
- IMM 5544: Resettlement Needs Assessment Form
- IMM 5725: Activities of Daily Living (ADL)
- IMM 5727: Global Assessment of Functioning (GAF)
- IMM 5728: Acknowledgment of HIV Post-Testing Counselling
- IMM 5733: Instructions for Pregnant Client − X-Ray Deferred
- IMM 5734: Specialist’s Referral Form
- IMM 5738: Chart of Early Childhood Development (CECD)
IMM 1017: Medical Report – Client Biodata and Summary

IMM 1017B Upfront: Upfront Medical Report – Client Biodata and Summary


IMM 5419 Medical Report






IMM 5544: Resettlement Needs Assessment Form


IMM 5725: Activities of Daily Living (ADL)

IMM 5727: Global Assessment of Functioning (GAF)

IMM 5728: Acknowledgment of HIV Post-Testing Counselling

IMM 5733: Instructions for Pregnant Client − X-Ray Deferred

IMM 5734: Specialist’s Referral Form

IMM 5738: Chart of Early Childhood Development (CECD)



Appendix IV: List of Immigration Medical Examination Instructions (IMEIs)
A) List of IMEIs related to process changes resulting from eMedical implementation
- IMEI: Activities of Daily Living Assessment (ADL)
- IMEI: Assessment of Cognitive Functioning
- IMEI: Body Mass Index (BMI)
- IMEI: Breast Examination
- IMEI: Developmental Milestones: Chart of Early Childhood Development (CECD)
- IMEI: Global Assessment of Function (GAF)
- IMEI: Height/Weight/Head Circumference Percentile for Children
- IMEI: Resettlement Needs Assessment (IMM 5544)
- IMEI: Serum Creatinine
- IMEI: Urinalysis
B) List of IMEIs related to conditions of significance
- IMEI: Cancer or Malignancy
- IMEI: Cardiac Disease
- IMEI: Cognitive Impairment in Adults
- IMEI: Debilitating Conditions
- IMEI: Developmental Delay in Children
- IMEI: Diabetes
- IMEI: Hearing Impairment or Deafness
- IMEI: Hepatitis/Liver Disease
- IMEI: HIV Screening
- IMEI: Hypertension
- IMEI: Psychiatric Conditions
- IMEI: Renal Disease
- IMEI: Syphilis Screening and Management
- IMEI: Tuberculosis
Appendix V: Instructions for Submission of Paper-Based IME
This appendix provides the order of the following various documents that are part of the IME:
- IMM 1017: Client Biodata and Summary or IMM 1017B Upfront – Client Biodata and Summary
- IMM 5743: Client Consent and Declaration
- IMM 5419: Medical Report: Medical History Questions
- IMM 5419: Medical Report: Physical Examination
- IMM 5419: Medical Report: Laboratory Requisition and Report
- IMM 5419: Medical Report: Chest X-Ray Requisition and Report
- Urinalysis Report(s)
- HIV Report
- Syphilis Report, RPR Report(s)
- Chest X-Ray Report – Radiology Findings
- All other medical reports
- Any other information (passports, visas, letters, etc.)
- Chest x-ray:
- Digital chest x-ray (DICOM) – Staple the top left of the CD envelope to the back of the IME, with the client’s name visible on either the envelope or the DICOM itself; or
- Chest x-ray in hard copy (if DICOM is not available). If possible, lateral x-rays should be placed upside down, with the spine on the left side, and stapled behind the IME on the top left corner. Frontal x-rays should be placed upside down with the left ventricle on the left side, and stapled behind the IME on the top left corner. Frontal x-rays are placed after lateral x-rays.
Include a log sheet with the client’s name and date of birth and the file numbers of all files in the package. The log sheet and tracking numbers are used to trace lost or misplaced records.